- Home
- Mental Health Concerns for New Parents
- About Perinatal Mood Disorders
Call the NJ Family Health Line
If you or someone you know is experiencing a pregnancy related mood disorder.
Call 1-800-328-3838
Helpline hours are Monday-Friday 8AM - 6PM
About Perinatal Mood Disorders
|
General Information |
Types of PMD |
The exact causes are unknown. Here are some factors that may contribute:
|
 |
Women need to know the signs and symptoms of perinatal mood disorders because early diagnosis is important. Husbands, partners, friends and family members can help. Often, they recognize a problem even before the woman herself does.
10–20% of women develop a mood disorder at some point from the time they become pregnant to up to a year after giving birth. Initially, research focused on postpartum depression (PPD) associated with the time after pregnancy, but behavioral scientists have since learned that many of these disorders might occur during pregnancy too.
Many physical and emotional changes occur before and after giving birth. Most women experience mixed and often contradictory feelings, but these feelings slowly go away.
However, when symptoms of sadness, anxiety, depression, frustration and other disturbing emotions persist and a mood disorder develops, professional health is often necessary.
All perinatal mood disorders are treatable. Read more about treatment options.
Ten percent of women experience depression during pregnancy and one in every eight to 10 women experiences postpartum depression (PPD) within the first year after childbirth, miscarriage or stillbirth.
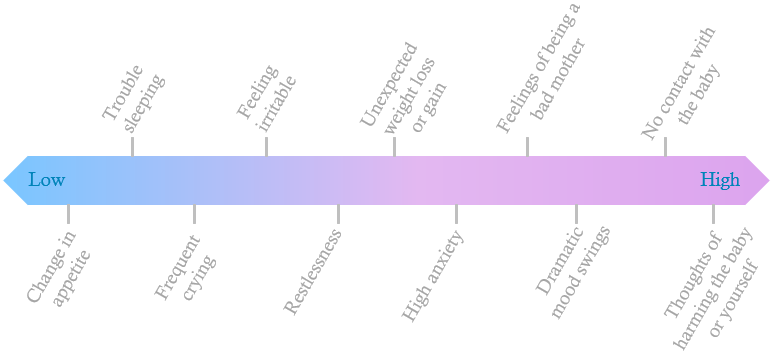
For common symptoms see scale for signs of PMD.
Approximately 6 percent of pregnant women and 10 percent of postpartum women experience anxiety, which can occur on its own or in addition to depression. Risk factors include a personal history of perinatal anxiety or depression, a family history of anxiety, or a thyroid imbalance.
Postpartum OCD occurs in approximately 3 – 5 percent of childbearing women.
- The most common obsession is thoughts or mental images of harming or even killing one’s own baby.
- The most frequent compulsion is bathing the baby often or changing the child’s clothes.
Mothers know these thoughts are bizarre and are highly unlikely to ever act on them. Risk factors include history of OCD and/or negative feelings about motherhood resulting from unrealistic expectations.
Approximately 10 percent of postpartum women experience panic disorder, which usually appears to come out of nowhere. Sufferers fear its return, causing anxiety. Risk factors include previous history of panic disorder and thyroid dysfunction.
Between 1 and 6 percent of women experience PTSD after childbirth. The cause is most often real or perceived trauma during childbirth such as:
- Unplanned C-section
- Health issues with the baby
- Feelings of powerlessness, poor communication, and lack of support and reassurance during the delivery
Risk factors include previous trauma, such as rape or sexual abuse.
Postpartum psychosis occurs in 1 to 2 of every 1,000 births. Onset is usually within two weeks to three months after birth. A 5 percent rate of suicide/infanticide is associated with postpartum psychosis.
Immediate treatment is crucial. Risk factors include previous postpartum psychosis or depressions; manic-depressive (bipolar) history; prenatal stressors such as low socioeconomic status and lack of a supportive partner or social support; obsessive personality traits; family history of mood disorder.