
In order to qualify for incentives under the New Jersey Medicaid Promoting Interoperability Program, providers must meet both a Medicaid provider type requirement and a Medicaid patient volume requirement. Additionally, the Medicaid provider cannot be “hospital based”, defined as 90% or more of the provider's encounters taking place at an inpatient or emergency room place of service/practice location.
Physicians/clinicians cannot participate in both the Medicare and Medicaid Promoting Interoperability Programs. For more information on the differences between the Medicare and Medicaid Promoting Interoperability Programs, click on this link: Medicaid vs. Medicare?
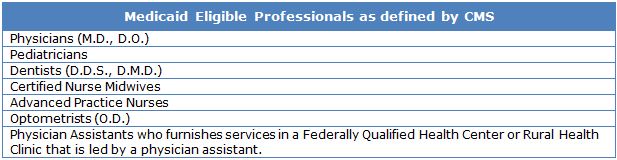
Provider Type Requirements
Only the specific types of Medicaid physicians/clinicians listed below are eligible to receive New Jersey Medicaid Promoting Interoperability Program payments.
Patient Volume Requirements
Eligible professionals that are not pediatricians must establish a 30% minimum Medicaid (Title XIX fee-for-service and managed care only) patient volume over any 90 day period in the most recently completed calendar year to be eligible for a New Jersey Medicaid Promoting Interoperability Program payment. Any attestations submitted for a calendar year 2015 Promoting Interoperability Program payment (available through March 31, 2016) should use patient volume from a 90 day period in calendar year 2014
Pediatricians will need to establish at least 20% Medicaid patient volume over any 90 day period in the most recently completed calendar year to be eligible for a 2/3 incentive payment. Pediatricians that establish a 30% Medicaid patient volume will receive a full incentive payment.
The only exception to the Medicaid patient volume is if a provider practices predominantly in a Federally Qualified Health Center (FQHC), defined at 50% or more a provider's total encounters over a six month period in the most recently completed calendar year having taken place in an FQHC. If this "practicing predominantly" condition is met, the provider can then show that 30% of their encounters were provided to "Needy Individuals", which include the following:
- Medicaid or CHIP clients;
- Patients furnished uncompensated care by the provider; or
- Furnished services at either no cost or on a sliding scale.
Additional information on New Jersey Medicaid EHR Incentive Program patient volume calculations can be found here.


