Contact the Rabies Unit
The Rabies Lab is open from 9:00am to 5:00pm, Monday through Friday. It is closed on weekends and holidays.
Email (preferred): rabies.PHEL@doh.nj.gov
NEW Phone: (609) 718-8366
Alt. Phone: (609) 530-8416
For emergency rabies testing, contact the Communicable Disease Service Rabies Lead at 609-826-4871.
Contact local Animal Control about suspicious animals around or in the house
Contact NJ Department of Agriculture Animal Pathology at 609-406-6999 or https://nj.gov/agriculture/ahdl/ for submission of livestock or agricultural animal heads for testing.
Did you know?
- The PHEL Rabies Unit tests about 3,000 animals each year
- Rabies occurs most often in wild animals
- Among domestic animals, cats are the most often positive
- Wild animals tested include raccoons, bats, skunks, groundhogs and foxes
- Among wild animals, raccoons are most often positive for rabies
- Fewer than one percent (1%) of bats carry rabies in New Jersey
- PHEL tests livestock and domesticated wild animals
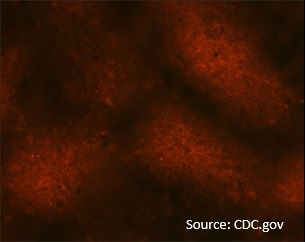
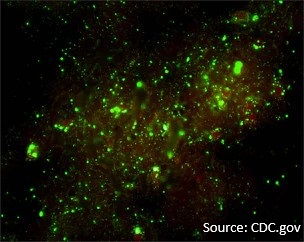
- The test for rabies is performed on animal brain tissue
- PHEL utilizes the Direct Fluorescent Antibody (DFA) method
- Rabies testing follows the CDC standardized testing protocol
- Highly trained laboratory personnel perform rabies testing
- Testing is done under strict bioSafety standards
- Sample handling and disposal follows WHO/CDC Standards