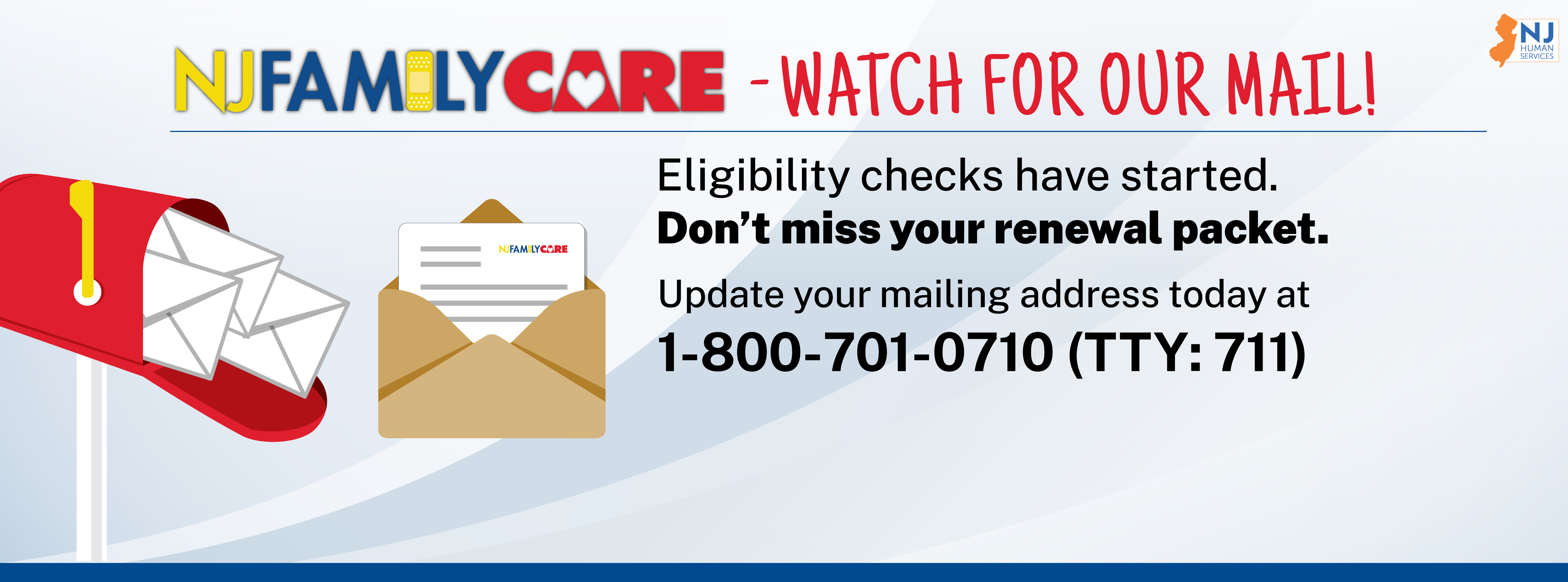
Call to update your address, and get ready to receive a renewal packet.
"Unwinding” is the process where New Jersey will restart yearly eligibility reviews for everyone enrolled in NJ FamilyCare/Medicaid. This started on April 1, 2023.
During the unwinding, NJ FamilyCare/Medicaid will send renewal packets for members to complete and return. Then NJ FamilyCare/Medicaid will decide if members still qualify for coverage. You can learn more about who can qualify here. Members who still qualify will keep their NJ FamilyCare/Medicaid coverage.
Members will know it is their time to renew when they get mail from the State of New Jersey or their County Board of Social Services. Members should open all letters, follow instructions, and respond right away to help stay covered.
Most people who have a managed care organization (MCO), also known as an HMO or a health plan, will also get a postcard from their plan. This means that their renewal packet is coming that month, and they should look for mail.
Some members will get calls from a Regional Health Hub or a New Jersey state employee to talk about their renewals.
Members should call NJ FamilyCare at 1-800-701-0710 (TTY: 711) if any of their information changes, like their phone number or mailing address.
Most NJ FamilyCare members will receive their renewal paperwork in the mail to the address in NJ FamilyCare’s files. To update or confirm an address, call 1-800-701-0710 (TTY: 711).
NJ FamilyCare members can call 1-800-701-0170 (TTY: 711) to get another renewal packet. Members who know the County Board of Social Services that manages their case can call their county office – a list of phone numbers is available here.
New Jersey resumed ordinary eligibility processes for everyone enrolled in NJFamilyCare/Medicaid on April 1, 2023. NJ FamilyCare has to check eligibility for over two million NJ FamilyCare members during the 12 months between April 2023 and March 2024.
- Call NJ FamilyCare/Medicaid at 1-800-701-0710 (TTY: 711) to update their contact information. This is especially important if they have moved in the last three years.
- Watch for mail from the State of New Jersey or your county, and make sure to reply on time to avoid a gap in coverage.
Members should allow at least 30 days before reaching out to NJ FamilyCare to ask questions about their renewal packet submission. If 30 days pass and they want an update, they can call their County Board of Social Services or NJ FamilyCare at 1-800-701-0710 (TTY: 711).
Members should also look for follow-up mail after submitting their renewal packet. If a member moves or gets a new phone number after submitting their renewal packet, it is important to let NJ FamilyCare know by calling 1-800-701-0710 (TTY: 711). If a member gets a letter, they should follow all instructions and send it back as soon as possible.
Technical Questions
Invitation codes are a series of numbers and letters that bring members to an individualized renewal application online. The invitation codes are included in the renewal mailing that many members receive in the mail. Members who receive the code can enter it at https://dmahs-nj.my.site.com/familycare/quickstart on the left side of the page.
The call center is open the following hours:
- Mondays from 8:00am to 8:00pm
- Tuesdays from 8:00am to 5:00pm
- Wednesdays from 8:00am to 5:00pm
- Thursdays from 8:00am to 8:00pm
- Fridays from 8:00am to 5:00pm
The wait time is currently higher than average to talk to a customer service representative. While we work to improve customer service in our call center, members can be advised that hold times tend to be less in the early morning and late afternoon, and on Mondays and Thursdays.
Visit the online application page. In the middle column, select “forgot password.” Follow the instructions to reset the password. For step-by-step instructions with illustrations, visit this link.
NJ FamilyCare is in the process of upgrading our systems so that applications and renewals are easily accessible on all platforms. At this time, Google Chrome and Microsoft Edge are the best internet browsers to use. Internet Explorer is no longer supported and may not work properly. Laptops and desktop computers are the best devices for completing renewals. Cell phones and tablets may be more challenging because the screens are smaller and will require scrolling and zooming in and out.
Parents and legal guardians can request coverage for themselves on their child’s renewal application. Other family members can also request coverage, including other children and adults who live together.
No. Beware of renewal scams. NJ FamilyCare will never charge or ask for money from members to enroll or re-enroll. Do not share banking or credit card information with anyone that calls you, claiming to represent NJ FamilyCare, the Department of Human Services, the Division of Medical Assistance and Health Services, or your NJ FamilyCare Health Plan. Don’t hesitate to call NJ FamilyCare at 1-800-701-0710 (TTY: 711) to report a scam or verify legitimate information. Flyers in 21 languages about scam and fraud awareness are available at https://njfamilycare.dhs.state.nj.us/use_benefts.aspx.
Additional Questions
Members should take time to make sure the renewal process goes smoothly by responding to requests for information and reporting changes in their household like pregnancy, address, income, and so on. Those members determined to be eligible will continue to receive NJ FamilyCare/Medicaid benefits.
If a member no longer qualifies for coverage through NJ FamilyCare/Medicaid, they may be referred to GetCoveredNJ, where they can get help paying for healthcare coverage. GetCoveredNJ is the state's official health insurance marketplace where individuals and families can easily shop for and buy affordable healthcare coverage.
A member who has lost coverage but believes they still qualify should call their County Board of Social Services or the NJ FamilyCare health benefits coordinator at 1-800-701-0710 (TTY: 711).
If a member has Medicare, they may qualify for help with premiums, co-pays, and deductibles through New Jersey’s Medicare Savings Programs. Learn more about program eligibility and benefits by calling 1-609-792-9745 (TTY: 711).
Members have 60 days to request a fair hearing. This is a special extension for the return to regular renewals.
Members can find information about COVID-19 at trusted sources like the New Jersey Department of Health and the Federal Centers for Disease Control.
New Jersey COVID-19 Information Hub
Where to get a COVID-19 Test in NJ
Where to get a COVID-19 Vaccine in NJ
Weekly COVID-19 Activity Reports
COVID-19 Information for Schools
- Advise NJ FamilyCare/Medicaid members to call 1-800-701-0710 (TTY: 711) to update their contact information. This is especially important if they have moved in the last three years.
- Share information about NJ FamilyCare/Medicaid changes and actions that members need to take to maintain NJ FamilyCare/Medicaid coverage.
- Check the Stay Covered NJ website frequently. This website is updated to reflect the most current FAQs and guidance.
- Download and share materials from the Stay Covered NJ Toolkit.
- Share information about NJ FamilyCare/Medicaid renewals in patient waiting areas, in clinical rooms, and in meetings. Hang posters and leave NJ FamilyCare information in common places.
- If an NJ FamilyCare/Medicaid member reports an updated address to the provider office, remind them to also call 1-800-701-0710 (TTY: 711) to update their address with NJ FamilyCare/Medicaid.
- Check the Stay Covered NJ website frequently. The Stay Covered NJ Toolkit is updated to reflect the most current guidance.
NJ FamilyCare/Medicaid is working with managed care organizations (MCOs), County Boards of Social Services, and community partners to
- raise awareness,
- encourage members to update their contact information, and
- encourage members to respond to all mail from NJ FamilyCare/Medicaid.
The five NJ FamilyCare Health Plans (Aetna, FidelisCare, Horizon NJ Health, United, and WellPoint) will send postcards at the beginning of each month to the 1/12th of members who will get their renewals that month. They will follow up later in the month by phone, email, and text message when possible. NJ FamilyCare/Medicaid is also working closely with GetCoveredNJ to ensure New Jerseyans have access to healthcare coverage even if they are no longer eligible for NJ FamilyCare/Medicaid.
 Official Site of The State of New Jersey
Official Site of The State of New Jersey