Healthy New Jersey
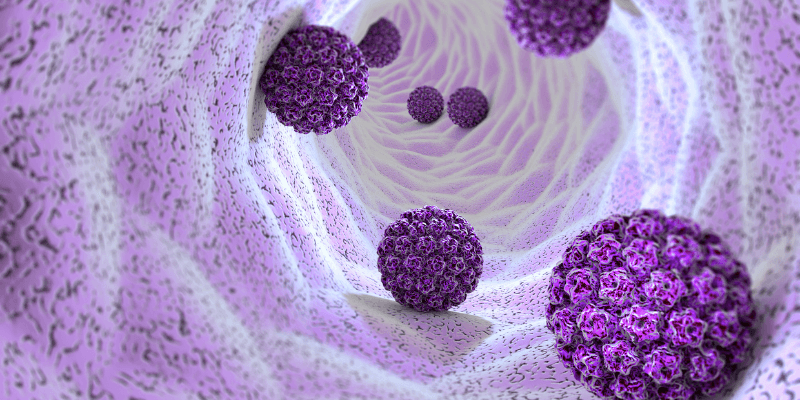
HPV
Human papillomavirus (HPV)
HPV is the most common sexually transmitted infection (STI) in the world. In fact, most sexually active people will get HPV at some point in their lives without even knowing it.
The good news? Most HPV infections go away on their own—but some types can cause genital warts or lead to cervical, anal, and other cancers. The best way to protect yourself is through vaccination, routine screening, and safer sex practices.
This page covers everything you need to know about HPV, including how it spreads, symptoms to watch for, and steps you can take to stay safe.
HPV Information
HPV is a group of more than 200 related viruses that spread through skin-to-skin contact. It is commonly transmitted during vaginal, anal, or oral sex, but you don’t need to have intercourse to get HPV—it can spread through any genital contact.
HPV infections fall into two main categories:
- Low-risk HPV – Can cause genital warts but does not lead to cancer.
- High-risk HPV – Can cause cervical, anal, penile, throat, and other cancers if the body does not clear the infection.
Most people with HPV have no symptoms and never experience health problems. However, some HPV infections persist and can lead to serious complications, making regular screening and vaccination essential.
Most HPV infections cause no symptoms and go away on their own within 1-2 years. However, some types of HPV can cause:
Genital Warts (Low-Risk HPV)
- Small, flesh-colored or gray growths in the genital or anal area.
- Warts can be raised, flat, or clustered (like cauliflower).
- They may cause itching, discomfort, or bleeding but are usually painless.
Cancer-Causing (High-Risk) HPV
Most high-risk HPV infections don’t cause symptoms until they lead to more serious conditions, such as:
- Cervical cancer – May not cause symptoms until it is advanced. Regular Pap smears help detect early changes in cervical cells.
- Anal, penile, vaginal, vulvar, and throat cancers – Symptoms depend on the location but may include pain, lumps, or unusual bleeding.
Because HPV often has no symptoms, regular screening is the best way to detect and prevent complications.
How Do You Get Tested for HPV?
For Women & People with a Cervix
- Pap Smear – Checks for abnormal cervical cells caused by HPV.
- HPV Test – Identifies high-risk HPV strains in cervical cells.
- Routine Screening – Recommended for people aged 25-65, typically every 3-5 years.
For Men and People Without a Cervix
- There is no routine HPV test for men or individuals without a cervix.
- Health care providers may check for HPV-related cancers (e.g., anal, penile, or throat cancer) during physical exams.
- If you have symptoms like genital warts or unusual lumps, see a doctor for evaluation.
When Should You Get Tested?
- If you’re 25 or older, ask your doctor about routine cervical screening.
- If you notice genital warts, unusual growths, or symptoms of throat cancer, seek medical evaluation.
- If you are at higher risk (e.g., weakened immune system, HIV-positive), talk to a health care provider about additional screening.
There is no cure for HPV, but most infections go away on their own. If treatment is needed, options depend on what type of HPV you have.
For Genital Warts (Low-Risk HPV)
- Prescription creams – Can shrink warts over time.
- Freezing (Cryotherapy) – A health care provider can freeze off warts.
- Laser or Surgical Removal – Used for larger or persistent warts.
For High-Risk HPV & Abnormal Cell Changes
- Cervical procedures (e.g., LEEP, cryotherapy) – If a Pap smear finds abnormal cells, treatment may be needed to prevent cervical cancer.
- Cancer treatment – If HPV leads to cancer, treatment will depend on the type and stage.
Even though HPV itself isn’t curable, its effects can be managed and prevented through vaccination and routine screening.
The HPV vaccine (Gardasil 9) is the best way to prevent HPV-related health problems. It protects against 9 types of HPV, including those most likely to cause genital warts and cancer.
Who Should Get the HPV Vaccine?
- Children & Teens (Ages 9-14) – The vaccine works best when given before exposure to HPV. Two doses are recommended.
- Young Adults (Ages 15-26) – If not vaccinated earlier, three doses are recommended.
- Some Adults (Ages 27-45) – The vaccine may still be beneficial. Talk to your health care provider.
Why Get Vaccinated?
- Nearly 100% effective at preventing HPV-related cancers and warts.
- Safe & long-lasting – Protection lasts for many years.
- Helps protect partners – Reduces HPV transmission.
If you haven’t been vaccinated yet, it’s never too late to ask your health care provider about your options.
- Use condoms and dental dams – While not 100% effective, they reduce HPV transmission risk.
- Get routine cervical screenings – Pap smears and HPV tests help catch early cell changes before they turn into cancer.
- Talk to your partners about HPV – Open communication about STI prevention is key.
- Consider the HPV vaccine – If you haven’t been vaccinated, it’s the best way to protect yourself.
Since HPV spreads through skin-to-skin contact, condoms do not provide full protection, but they lower your risk significantly.
Most HPV infections do not affect pregnancy, but some risks exist:
- Genital warts can grow larger due to hormonal changes.
- High-risk HPV can cause cervical cell changes that require monitoring.
- Rarely, HPV can be passed to the baby, causing a throat condition called recurrent respiratory papillomatosis (RRP).
What Can You Do
- Get screened for HPV before pregnancy.
- If you have HPV, inform your doctor so they can monitor for complications.
- HPV does NOT affect fertility, but abnormal cervical changes may require treatment before conception.
HPV is common in pregnancy, and most cases do not cause serious problems. However, regular check-ups help ensure a safe pregnancy and delivery.

Take Charge of Your Health
- Get vaccinated if you haven’t already
- Schedule routine screenings (Pap & HPV tests)
- Use protection & talk to partners about STI testing
 Official Site of The State of New Jersey
Official Site of The State of New Jersey