Since March of 2020, NJ FamilyCare/Medicaid has followed special rules related to the federal COVID-19 Public Health Emergency (PHE). These rules have allowed most NJ FamilyCare/Medicaid members to keep their health coverage, even if they no longer qualified – for example, if their income was too high. However, Congress passed legislation that said state Medicaid programs had to go back to following normal federal rules as of April 1, 2023.
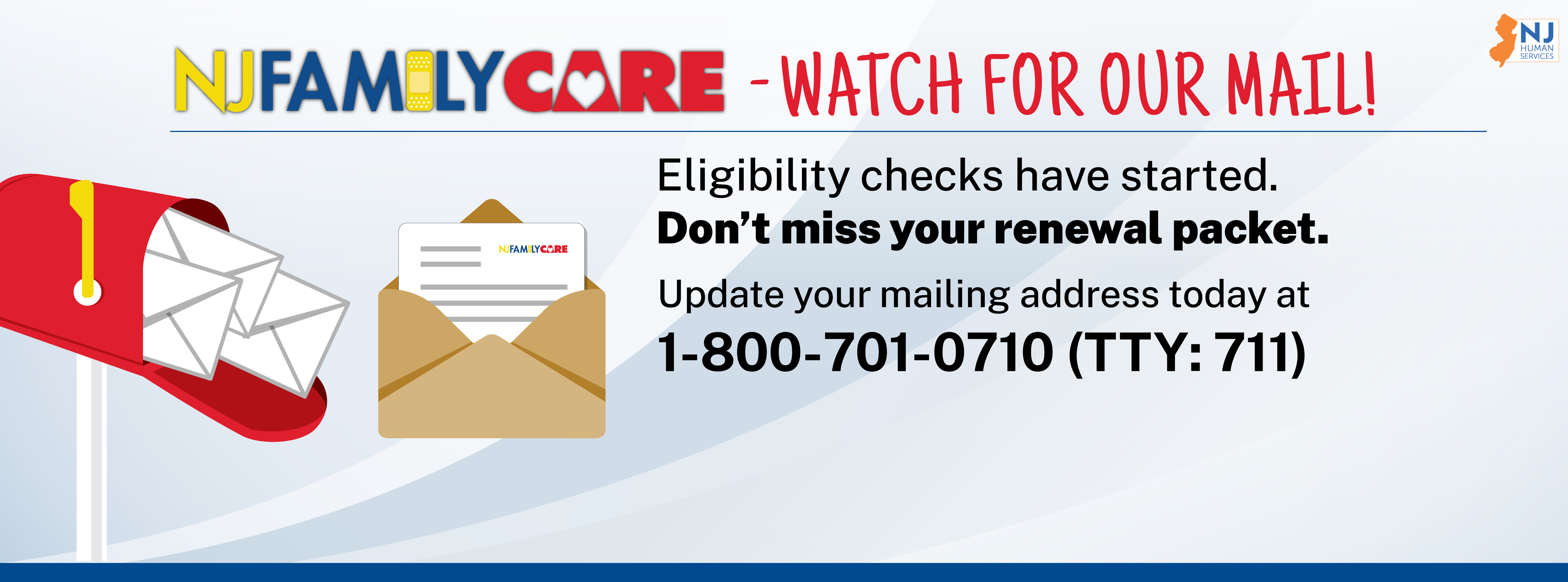
NJ FamilyCare has re-started eligibility reviews. This means that all members enrolled in an NJ FamilyCare program will be reviewed to see if they still qualify for coverage. As part of this review, many members will receive mail from the State of New Jersey or their County Board of Social Services. Members will have to provide or confirm additional information so NJ FamilyCare/Medicaid can decide whether they still qualify for healthcare coverage. Members who do not respond to NJ FamilyCare/Medicaid mail may lose their coverage.
Videos about the Return to Regular Renewals
Eligibility Unwinding Progress
MAAC meeting
The April meeting of the Medical Assistance Advisory Council (MAAC) featured a discussion of the unwinding process with stakeholder feedback. Watch the presentation, or read the slide deck.
MCO partnerships
New Jersey’s five managed care organizations (MCOs) are working with NJ FamilyCare/Medicaid to share updated member contact information, reach out to members who have not responded to NJ FamilyCare mail, and help members avoid disenrollment. At the beginning of each month, MCOs will send postcards to members who are going to get their renewal mail that month. Learn more on the “Members: Renew” tab above.
Sharable documents
NJ FamilyCare has prepared documents that providers and community-based organizations can print and share. Find these resources in the “Stay Covered NJ Toolkit” tab above.
Transition to other coverage
People who no longer qualify for NJ FamilyCare may be able to get health coverage through GetCoveredNJ, the State’s official health insurance marketplace. GetCoveredNJ offers immediate eligibility results and says if people can get help lowering the cost of their monthly premiums. After reviewing their results, people who are eligible for Marketplace coverage can compare options and enroll in a Marketplace plan that best meets their needs.
 Official Site of The State of New Jersey
Official Site of The State of New Jersey